Muscular dystrophy (MD) is a grouping of several medical conditions rather than a singular disease in itself. The common factor among the conditions in this group is a progressive loss of both muscle and strength in the body. We are going to provide you with a list of some of the essential facts to know about MD and what therapies are available to get help, such as activity-based therapy. These are the topics we will consider:
- Conditions that are considered muscular dystrophy
- Symptoms of Muscular dystrophy (including early warning signs)
- Getting a diagnosis for muscular dystrophy
- The primary cause of Muscular dystrophy
- Therapies for slowing the progress of muscular dystrophy (there is currently no known cure)
When you hear about muscular dystrophy, it is usually Duchenne, the most common condition in this group of diseases. In fact, we will discuss the symptoms associated with Duchenne in the next section. However, it is vital to know that there are other conditions in this grouping. Here are several of them, along with a little bit about what sets them apart.
- Becker – The symptoms of Becker are similar to Duchenne except for the fact that the disease usually begins later and progresses slower. Therefore, life expectancy with Becker is into a person’s 40s (as opposed to in their 20s with Duchenne).
- FSHD – Onset is usually during the teen years. Muscle weakness often begins in the face and shoulders. It can be difficult for a patient to close his or her eyelids fully and they may sleep with the lids partially open. Shoulder blades protrude sharply in a wing-like shape when a patient raises their arms over their head.
- Limb-girdle – The onset can be in the teen years or younger. The pelvis and shoulders are the first regions affected. The patient may also trip frequently due to a very specific problem with raising the front half of the foot.
- Myotonic – This is the most common form of Muscular dystrophy when the onset happens after a person is already an adult (but onset can also be younger). The condition name stems from its main symptom – myotonia. It means that contracted muscles do not relax naturally as they should. Symptoms usually begin in the face and neck.
While these are not the only conditions that MD includes, it gives you an idea of the broadness and diversity of the diseases within this grouping.
Symptoms of Muscular Dystrophy in Children
Some children can receive a diagnosis of MD as early as age three due to the notability of some of the early symptoms. A few early warning signs to watch out for include:
- Walking issues – These can include waddling when walking, frequent falling, or walking on the toes. In less severe cases, the patient may just have problems with jumping or running at first.
- Sit/stand problems – Changing positions from lying down to sitting to standing may be difficult to coordinate due to muscle weakness or pain.
- Muscle pain – Stiffness and soreness may be chronic early on.
- Learning disabilities – MD patients can experience some learning disabilities and may not begin to speak until much later.
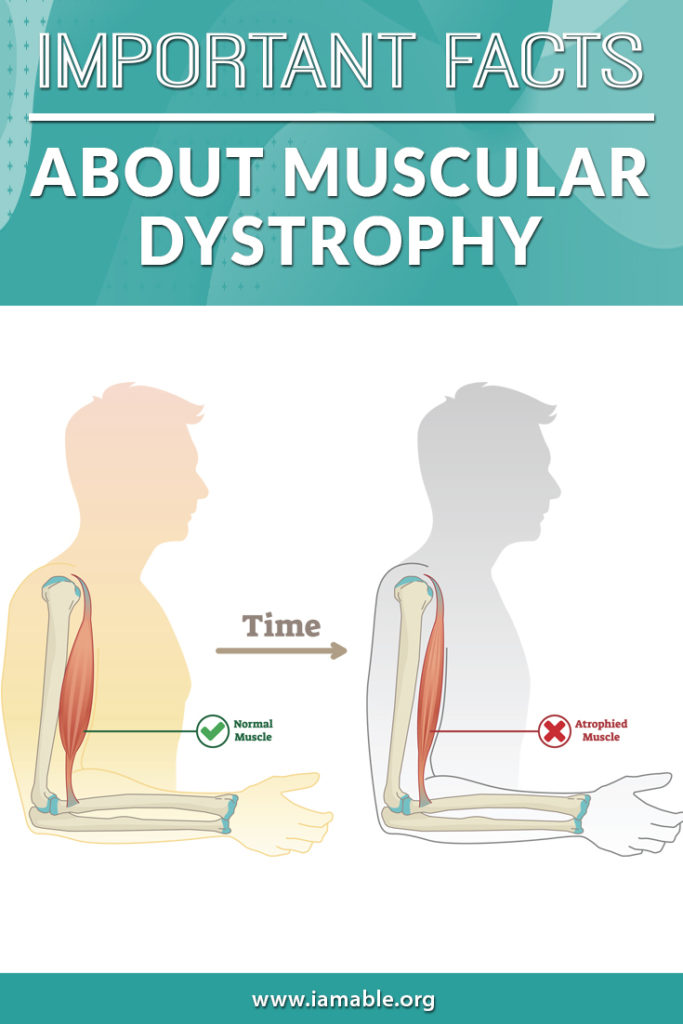
Unfortunately, these symptoms may progress rather rapidly depending on how early the condition is caught, the level of care, and the severity of the disease. Once MD is full-blown, symptoms will include loss of ability to walk, muscle atrophy, breathing issues that may require assisted breathing, extreme curvature of the spine (due to the inability of the surrounding muscles to provide support), heart problems (remember that the heart is a muscle), and difficulty swallowing that may eventually require a feeding tube.
Getting a Diagnosis Can Be a Long Process
Why is this the case? There is no single definitive test to reveal if a person has MD or not. The first thing a doctor may do, if symptoms present, is to ask about family history to see if MD runs in the family. Tests can rule out other possibilities. There are some tests that clearly indicate a problem with the muscles.
For example, serum creatine kinase in the blood may indicate that muscle fibers are breaking down at an abnormal rate. Of course, this does not mean that it is MD causing the damage, but if the diagnosis is suspected, this can increase the likelihood.
Muscle biopsies and DNA checks can also provide indicators of MD. The body needs dystrophin to maintain muscle shape and length, so low levels revealed by the biopsy could indicate MD. In the end, a combination of test results, symptoms, and family history will help your doctor to make a diagnosis.
The Primary Cause of MD is a Chromosome Mutation
Depending on the type of MD, there will be different mutations on the X chromosome. This is why a DNA test may shed light on the diagnosis and cause. However, it is crucial to understand that there are over 1,000 different possible mutations that relate to muscular dystrophy.
Progressive Muscle Weakness and How Muscular Dystrophy Affects Daily Life
One of the defining characteristics of muscular dystrophy is progressive muscle weakness. This means that, over time, the muscles affected by the disease continue to weaken and deteriorate. The extent of muscle weakness and the specific muscles affected can vary depending on the type of MD. As MD progresses, it can significantly affect daily life by making it difficult to perform everyday tasks such as walking, getting up from a seated position, or climbing stairs. Additionally, MD may impact respiratory function, heart health, and swallowing, which can lead to further complications and challenges in daily living. Early intervention, therapy, and supportive care can help manage these symptoms and improve the quality of life for individuals with muscular dystrophy.
3 Facts About Muscular Dystrophy You May Not Know
- Muscular Dystrophy Affects Both Men and Women Although some forms of MD, such as Duchenne and Becker, are more common in males due to their X-linked inheritance pattern, other types like FSHD and Limb-girdle muscular dystrophy can affect both men and women. The prevalence of MD varies depending on the type, but overall, it is estimated to affect 1 in every 3,500 to 6,000 individuals.
- There Are Over 30 Types of Muscular Dystrophy While the blog post has already mentioned some of the more common types of MD, it is essential to note that there are over 30 different types, each with its unique characteristics, symptoms, and progression. Some rare types of MD include Emery-Dreifuss, Oculopharyngeal, and Distal muscular dystrophy.
- Research Is Continuously Evolving to Improve MD Treatment Although there is no known cure for MD, scientists and researchers are continually working to improve treatments and therapies. Gene therapy, stem cell research, and new medications are some of the promising areas of research that may lead to better treatment options for MD patients in the future.
Muscular Dystrophy Symptoms in Adults
While many forms of MD have an early onset during childhood, some types of MD can present symptoms in adulthood. Adult-onset MD may include Myotonic dystrophy, Oculopharyngeal muscular dystrophy, and some forms of Limb-girdle muscular dystrophy. Symptoms in adults can vary greatly but may include:
- Muscle weakness, particularly in the face, neck, and limbs
- Difficulty swallowing or speaking
- Respiratory muscle weakness, leading to shortness of breath
- Cardiac issues, such as arrhythmias and cardiomyopathy
- Myotonia, or difficulty relaxing contracted muscles
- Fatigue and reduced exercise tolerance
Duchenne Muscular Dystrophy Interesting Facts
- Carrier Women Can Pass Duchenne Muscular Dystrophy to Their Children Since Duchenne muscular dystrophy is an X-linked recessive genetic disorder, carrier women have a 50% chance of passing the affected gene to their sons, who will have the condition, and a 50% chance of passing the carrier status to their daughters.
- Steroid Treatment Can Improve Outcomes for Duchenne Patients Corticosteroids, such as prednisone and deflazacort, can help slow the progression of muscle weakness and improve muscle strength in individuals with Duchenne muscular dystrophy. Steroid treatment is not a cure, but it can help maintain mobility and delay the onset of severe symptoms.
- Early Intervention is Crucial for Duchenne Patients The earlier a child is diagnosed with Duchenne muscular dystrophy, the sooner interventions such as physical therapy, occupational therapy, and medications can be implemented. Early intervention can help delay the progression of the disease and improve the quality of life for affected individuals.
Treating Respiratory Muscle Weakness in Muscular Dystrophy
As MD progresses, respiratory muscle weakness can become a significant concern for patients. To address this issue, healthcare providers may recommend:
- Breathing exercises and pulmonary rehabilitation to maintain lung function and improve breathing efficiency
- The use of non-invasive ventilation (NIV) devices, such as BiPAP or CPAP machines, to support breathing during sleep or periods of fatigue
- Monitoring lung function regularly to assess the need for additional respiratory support or interventions
- In severe cases, invasive ventilation via tracheostomy may be necessary to support breathing
Becker muscular dystrophy (BMD) is a milder form of MD that shares many similarities with Duchenne muscular dystrophy. However, BMD has a later onset and slower progression, which leads to a longer life expectancy for affected individuals. Here are some key points about Becker muscular dystrophy:
- BMD Onset: While Duchenne muscular dystrophy usually becomes apparent during early childhood, Becker muscular dystrophy typically has a later onset, with symptoms appearing during adolescence or early adulthood.
- Slower Progression: The progression of muscle weakness and loss of function is slower in Becker muscular dystrophy than in Duchenne, allowing individuals with BMD to maintain their mobility and independence for a longer period.
- Life Expectancy: People with Becker muscular dystrophy generally have a longer life expectancy than those with Duchenne, often living well into their 40s or beyond. With proper management and care, some individuals with BMD can live relatively normal lives.
- Treatment Approaches: Similar to Duchenne, there is no cure for Becker muscular dystrophy, but treatment focuses on managing symptoms, maintaining mobility, and improving the quality of life. Physical therapy, occupational therapy, medication, and assistive devices can all be beneficial for individuals with BMD.
While muscular dystrophy is a complex and diverse group of conditions, understanding the different types, their symptoms, and available treatment options can help patients and caregivers better manage the disease. With ongoing research and advancements in the field, there is hope for improved therapies and, eventually, a cure for muscular dystrophy.
There Is No Cure for MD, but Activity-Based Therapy May Help
Assistive devices can help children to attain a degree of independence and self-reliance despite living with a degenerative condition. Bracing can help the joints to stay healthy as long as possible. This is especially important once the surrounding muscle begins to degenerate.
Physical therapy, and particularly activity-based therapy, is crucial for maintaining the muscle as long as possible. The longer you can keep the muscles healthy, the more you can slow the progression. If you live in south Florida, iAM ABLE is the activity-based therapy center for you or your loved one. Schedule a consultation now, and download our eBook, which is especially beneficial for patients experiencing paralysis as the condition progresses.
Grab our free e-book 7 Unbelievably Important Steps to Take to THRIVE after Paralysis by clicking the image below.